
Summary:
Comorbidities and aging can have a significant impact on workers’ compensation claims. The aging workforce in the United States, combined with medical inflation and the higher possibility of comorbidity in older workers, is a driving factor in rising claim costs. Workers’ compensation payers can mitigate these challenges by being alert to the complex nature of preexisting conditions in an older workforce.
Aging Workforce:
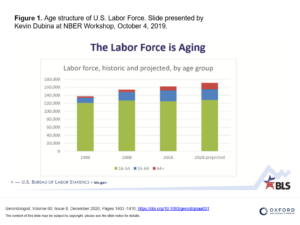
For a variety of reasons, the workforce in the U.S. is aging rapidly, and this trend is expected to continue [see chart].
People are living longer and healthier lives, leading to an increase in the number of older individuals who continue to work past the traditional retirement age. The U.S. Bureau of Labor Statistics (BLS) projects that in 2028, 25.2% of the national workforce will be aged 55 or older.[1] As the number of older individuals in the workforce increases, employers need to be aware that the potential for workers’ compensation claim quantity and severity is also likely to increase.
Aging Workforce Means More Comorbidities:
As our national workforce increases in age, there is a higher occurrence of pre-existing comorbidities. The most common comorbidities in workers of all ages in the U.S. include hypertension, drug abuse, diabetes, COPD, and obesity. Older workers, in particular, are more susceptible to certain comorbidities like:
- Diabetes
- Heart disease
- Mental health issues
If an older worker also has a comorbid diagnosis, that worker will likely have a more complicated and slower recovery, causing the worker to lose more time from work. According to Mary Beth Pittinger, Executive Vice President of Workers Compensation at Chubb Ltd., aging workers are more susceptible to having comorbidities which can contribute to an increase in the severity of a workers’ compensation injury. “A slower healing process, more complex and expensive treatments, and longer time away from work can all result when a worker with a comorbidity gets injured,” she said.[2]
Do Comorbidities Directly Affect Workers’ Compensation Claims?
Unfortunately, workers’ compensation claims that carry comorbidities, whether pre-existing or occurring after the injury, have been shown to be more serious and longer lasting. That, in turn, makes them more expensive for payers. And the occurrence of claims with comorbidity conditions is also on the rise.
According to a study conducted by the National Council on Compensation Insurance, workers’ compensation claims involving comorbidities have nearly tripled since 2000. Further, the average cost of workers’ compensation claims connected to a comorbid condition totals almost twice as much as that of comparable claims that don’t involve comorbidities.[3]
To sum up, comorbidities can significantly impact workers’ compensation claims in several ways:
- Increased claim duration and costs
- Delayed recovery: For example, if an injured employee is obese, the recovery time is typically longer.
- Increased risk of injury: For instance, hypoglycemia associated with diabetes can lead to falls and accidents.[4]
- Complications in treatment: For example, uncontrolled hypertension may increase cardiac risk, especially if procedures or operations are needed.[5]
How Can Payers Reduce the Effect of Comorbidities in Workers’ Compensation Cases?
To manage the impact of comorbidities, employers should get in front of the problem. Payers should encourage employees to manage any conditions they have through employee wellness programs. These programs can help by promoting healthy habits and improving overall well-being. This will increase the likelihood that pre-existing comorbidities will play only a minor role in recovery should a workplace injury occur.
In addition, organizations responsible for managing claims should consider the following strategies:
- Prevent and Identify Comorbidity: Payers should implement tools and strategies to proactively identify and manage these claims. This could include health screenings at the time of injury to identify any preexisting conditions that could affect the employee’s recovery time.
- Assign a Nurse Case Manager: A nurse case manager with experience in identifying comorbidities can be assigned to the case to determine if there are preexisting conditions that could affect the employee’s recovery time.
- Understand the Impact of Comorbidity: Understanding the contribution of both pre- and post-injury comorbidity is important for workers’ compensation payers due to significant impact on the cost and duration of claims.
- Be Aware of Common Comorbid Conditions: The five most common comorbid diagnoses identified in the workers’ compensation transactions study include hypertension, drug abuse (inclusive of alcohol and tobacco), diabetes, chronic pulmonary conditions, and obesity. Heart disease and mental health issues are sometimes listed as common cormorbid diagnoses for older workers.
- Collaborate with Healthcare Providers: Collaborating with healthcare providers to manage the treatment of workers with comorbidities can help ensure that the treatment for the work-related injury is not complicated by the comorbid condition.
Remember, each case is unique and the approach might need to be customized based on the individual’s health condition and the nature of the job. But, it benefits both the employer and worker to work with their managed care partner to identify and manage comorbidity conditions in advance of any injury or illness. Protecting and caring for employees up front can reduce the impact on severity, lost-time, and overall cost of workers’ compensation claims.
Please contact us if you have any questions on managing comorbidity conditions in injured workers.
[1] Clark, R. L., & Ritter, B. M. (2020). How are employers responding to an aging workforce? (Working Paper No. 26633). National Bureau of Economic Research. Retrieved from http://www.nber.org/papers/w26633
[2] https://www.businessinsurance.com/article/20220503/NEWS08/912349505/Severity,-cost-of-comp-claims-on-the-rise – :~:text=“In many cases, aging workers are more susceptible,executive vice president, workers compensation, at Chubb Ltd.)
[3] https://www.njda.org/news-information/news-archive/2020/11/09/work-comp-insights-the-impact-of-comorbidities-on-workers’-compensation-programs
[4] https://ama-guides.ama-assn.org/newsletter/article-abstract/24/5/8/95/Comorbid-Conditions-in-Workers-Compensation?redirectedFrom=fulltext
[5] https://ama-guides.ama-assn.org/newsletter/article-abstract/24/5/8/95/Comorbid-Conditions-in-Workers-Compensation?redirectedFrom=fulltext



